Immunotherapy – the revolution in cancer treatment
- Anson

- Nov 19, 2021
- 4 min read

Faced with long-term illness, one learns to reflect a lot about the past, including the recent past. But even I’m astonished that, despite blogging about cancer for the past 18 months, I never considered immunotherapy, although it has revolutionised cancer treatment over the past decade.
Immunotherapy is not new; it dates back more than 100 years. In the decades prior to 2011, immunotherapy treatments were geared towards the use of small proteins called cytokines (e.g. interferon) that were able to fight cancer by boosting the immune system and interfering with the way that cancer cells grew. Interferons, first manufactured in the 1980s, were also extensively used to treat viral infections (including hepatitis C) and multiple sclerosis. In 2011, however, a new drug called ipilimumab proved successful in controlling advanced skin cancer. This drug paved the way for the immunotherapy revolution that was to come.
tl:dr a new generation of immunotherapy drugs stop cancer cells from being able to hide from your immune system

Your immune system is highly complex and multifaceted. To be honest, my head still hurts trying to understand its complexities, and memories of failing Physiology 3H at Edinburgh University came flooding back!
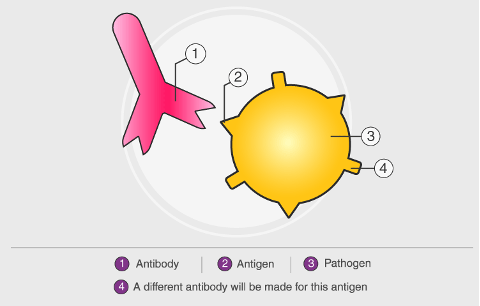
One of the many ways your immune system works is to produce white blood cells called T-cells (a type of lymphocyte) that kill specific foreign bodies (e.g. viruses and bacteria). They also kill cells that show uncontrolled growth, such as cancer cells and tumours. T cells have on their surface, proteins called antibodies that recognise surface proteins on foreign bodies called antigens, marking them for destruction.
Cancer cells produce tumour antigens, but they have also developed ways to escape detection, allowing unhindered growth. How do they do this? Well, in general, your body must prevent your immune system from not attacking healthy cells. One mechanism is called ‘negative regulation’ (and this is where my head starts to hurt, but stick with me!) via what are called ‘immune checkpoints’.
How to put the break on your immune system
T cells also have other special protein receptors on their surface called checkpoints that bind onto equally special proteins (called partner proteins) on the surfaces of other cells. Binding of checkpoint proteins to partner proteins acts as a check (or break) on your immune system, because when this binding takes place, a signal is sent to the T cell to turn itself off, and therefore not attack the cell it has just bound to. The particularly sneaky thing about cancer cells is that many of these also have partner proteins on their surface, turning off T cell activity, thereby allowing cancer cells to hide from the body’s immune system.
This is where the new immunotherapy drugs called ‘immune checkpoint inhibitors’ (ICI) come into play.
Imagine a drug that can prevent the binding of T cells checkpoint proteins to partner proteins on cancer cells.
If that is prevented, then no signal is sent to the T cell to turn itself off, and instead the T cell remains active, and able to kill the cell it has just bound to.
Basically the immune checkpoint is inhibited, allowing the immune system to be modified to improve its targeting in killing off cancerous cells.
Even more basically, the cancer cells can no longer hide from the body’s immune system.
I really recommend watching this short video as it explains really nicely how T cells recognise cancer cells, but also how cancer cells can evade detection through signalling to immune checkpoints. However, the types of stop signals that can come from cancer cells are many, and this is where different checkpoint inhibitor drugs are being developed, each targeting these different signals. And this is where my involvement with immunotherapy begins, and with a drug called pembrolizumab, or pembro between friends. It is also commonly known as Keytruda, its brand name.
Pembrolizumab
Technically, pembrolizumab is a monoclonal antibody. Pembrolizumab as a name is complicated (!) but follows convention to identify the type of drug and what it does:
Pembro- this is the prefix of the generic name, and I assume chosen by the scientists who developed the drug
-li- = shows that this drug is targeted at the immune system.
-zu- = identifies that the source of these antibodies were generated / cloned from non-human species (often mice or rabbits), but whose protein sequences have been modified to make them more human-like (i.e. humanized antibodies)
-mab = monoclonal antibody whose receptor targets are over-expressed on the outside of cancer cells
When I had my tumour biopsied, one of the tests they did was to look for a receptor protein on the surface of my cancer cells called PD-L1, short for ‘programmed death-ligand 1”. This is the partner protein of the checkpoint protein PD-1 present on the surface of the T cells (see figure below). Block the connection between PD-1 and PD-L1, and you block, or inhibit, this particular checkpoint.
Pembro was one of the first anti–PD-1 checkpoint inhibitor drugs to be developed (the other being nivolumab) and was initially licensed in 2014 to treat metastatic and advanced melanomas (skin cancer). Its use in the USA for Head and Neck Squamous Cell cancers was approved in 2016, and in the UK pembro was approved by NICE at the end 2020 for metastatic head and neck cancers. Its use is now extensive for many cancer types, but its development and history is fascinating.

So I’m hopeful that the treatment will work. I started immunotherapy treatment at Barts on Tuesday 16th November, and will receive an infusion of pembro every 6 weeks. But while the list of possible side effects is long and unpredictable, they are way, way less immediate than the chemotherapy I’d likely have started if my diagnosis had been only a year ago. And for that, I am very, very grateful.




It is so fantastic that this immunotherapy has become available in time to treat your cancer, Ans. Our daughter is undertaking her PhD studies at Barts Cancer Institute on this very same cancer immunotherapy research, so I am proud that her research is contributing to your treatment, the science of which I have also been getting my head around! Your blog is poignantly helping her understand the people this research benefits. It is excellent that you are embracing "science the s**t out of this" positivity and we will follow this with boundless hope for your recovery
Is it weird to look forward to reading these posts? Probably yes, as they chart a terrifying and perilous voyage. But Anson also makes the obscure and oft avoided technicalities of cancer so clear and accessible that it also feels as if that same light and precision is being brought to bear on the disease itself. And in this case it seems it really is : Go Pembro The Destroyer! Plus watching all those olives and Ferrero Rochers zipping around is also strangely soothing. Is that also weird, probably.